Pediatric Gastrointestinal Surgery
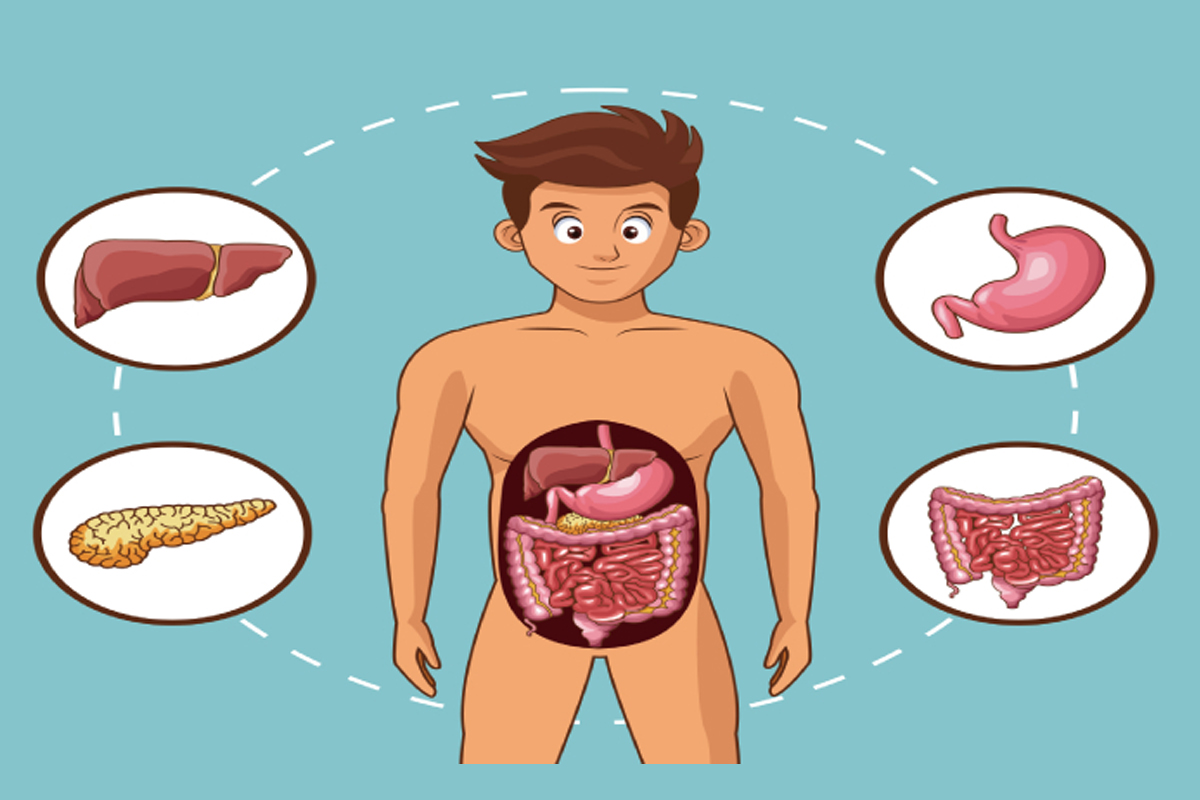
Pediatric Gastrointestinal Surgery
Pediatric gastrointestinal surgery is a specialized field of surgery that focuses on the diagnosis and treatment of gastrointestinal (GI) conditions in infants, children, and adolescents. It encompasses a wide range of surgical procedures involving the digestive system, from the esophagus to the rectum. Pediatric gastrointestinal surgeons are highly trained to provide surgical care for a variety of conditions that affect the GI tract in children. Here are some key aspects of pediatric gastrointestinal surgery:
-
Common Conditions: Pediatric gastrointestinal surgeons treat a variety of conditions, including but not limited to:
- Congenital Anomalies: Conditions present at birth, such as esophageal atresia, tracheoesophageal fistula, and intestinal malrotation.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn's disease and ulcerative colitis that can affect the intestines.
- Appendicitis: Inflammation of the appendix, which may require surgical removal (appendectomy).
- Gastroesophageal Reflux Disease (GERD): Chronic acid reflux that can lead to complications like esophagitis or hiatal hernias.
- Hirschsprung's Disease: A congenital condition that affects the large intestine's ability to move stool.
- Abdominal Tumors: Surgical removal of tumors or masses in the abdominal area.
-
Minimally Invasive Surgery: Many pediatric gastrointestinal surgeries can now be performed using minimally invasive techniques, such as laparoscopy or robotic surgery. These approaches offer smaller incisions, less postoperative pain, and quicker recovery times for children.
-
Nutritional Support: Pediatric patients with gastrointestinal conditions may require specialized nutritional support. Surgeons and nutritionists work together to ensure children receive the necessary nutrients, either through oral intake, enteral feeding (e.g., feeding tubes), or parenteral nutrition (intravenous nutrition).
-
Multidisciplinary Care: Pediatric gastrointestinal surgeons often collaborate closely with other healthcare professionals, including pediatric gastroenterologists, radiologists, nurses, and pediatric anesthesiologists, to provide comprehensive care to young patients.
-
Long-Term Follow-Up: Some gastrointestinal conditions require ongoing management and follow-up care. Pediatric surgeons may work with patients and their families to monitor progress, adjust treatment plans, and address any potential complications.
-
Patient-Centered Care: Given the unique needs and developmental stages of pediatric patients, pediatric gastrointestinal surgeons are trained to provide compassionate, child-friendly care. They work to minimize the psychological and emotional impact of surgery on children and their families.
-
Research and Advancements: Pediatric gastrointestinal surgery continues to benefit from ongoing research and advancements in surgical techniques, anesthesia, and postoperative care. This helps improve outcomes and reduce the invasiveness of procedures.
-
Pediatric Surgeon Qualifications: Pediatric gastrointestinal surgeons are typically board-certified in pediatric surgery and may have additional training or experience in pediatric gastroenterology and hepatology. They undergo rigorous education and training to ensure they can provide specialized care to children.
It's important for parents or caregivers to work closely with healthcare providers to understand the treatment options available for a child with a gastrointestinal condition. Pediatric gastrointestinal surgeons play a crucial role in providing surgical solutions when necessary and ensuring the best possible outcomes for pediatric patients.